ISSN (O):2395-2822; ISSN (P):2395-2814
Recurrent Choledochal Cyst with Pancreatitis – A Rare Indication for Whipple’s Surgery
– Case Report and Review of Literature.
Rohan Reddy C1, Parag W Dhumane2, Prasad K Wagle2, Sadanand B Shetty2
1Resident, General Surgery, Lilavati Hospital, Mumbai.
2Consultant, General Surgery, Lilavati Hospital, Mumbai.
ABSTRACT:
A young man presented to us with a history of repeated episodes of epigastric pain, he was evaluated and diagnosed of recurrent pancreatitis. Imaging revealed a choledochal cyst arising from the infra duodenal portion of common bile duct and pancreatic duct opening into it. The choice of surgical intervention in choledochal cysts has always been debated, especially in cases with such anatomy. In the following case report we briefly describe the operative method and rationale for our choice.
INTRODUCTION:
Choledochal Cyst is a rare congenital dilatation of the bile ducts. The estimated incidence in Western countries varies between 1 in 100,000 and 1 in 150,000[1] The incidence is higher in Asia and occurs more in women, with a male to female ratio of 1:3 to 4.[1,2] In 1723, Vater was the first to show a fusiform dilation of the common bile duct and Douglas published on the possible congenital origin of this cyst in 1852.[3-4]
We describe the case of a young man with recurrent choledochal cyst, who required Whipple’s procedure as a definitive surgical treatment.
CASE REPORT:
A 30 yr old gentleman presented to us with a 2- month history of episodic, severe upper abdominal pain, that was maximum on the day of admission. He had several episodes of non-bilious vomiting over the same period. The patient was hemodynamically stable, significant tenderness was noted in the epigastric region associated with voluntary guarding. There was no evidence ascites or organ dysfunction. The patient gives a history of an abdominal surgery done for a ‘cyst/mass’, when he was 12 years old. Reportedly, he had undergone partial excision of the cyst and gall bladder removal. However, no medical records were available with the patient.
On admission, he had leucocytes of 13,400/cc and had a normal liver panel. Sr. Amylase and Sr. Lipase were grossly elevated at 881 U/L and 2385
U/L, respectively. He had undergone a EUS before presenting to us, which revealed a cystic lesion close to the head of pancreas filled with debris and a patent hepatico-duodenostomy [Figure 1]. A CECT abdomen was done on admission that confirmed the pathology [Figure 2]. MRCP revealed the pancreatic duct opening into the cyst arising from the infra-duodenal portion of CBD. [Figure 3]. The patient was thus, diagnosed of recurrent choledochal cyst with acute pancreatitis. Any surgical intervention was deferred in view of active organ inflammation, hence he was conservatively managed until the symptoms settled and was discharged home. He was admitted after one month for surgery.
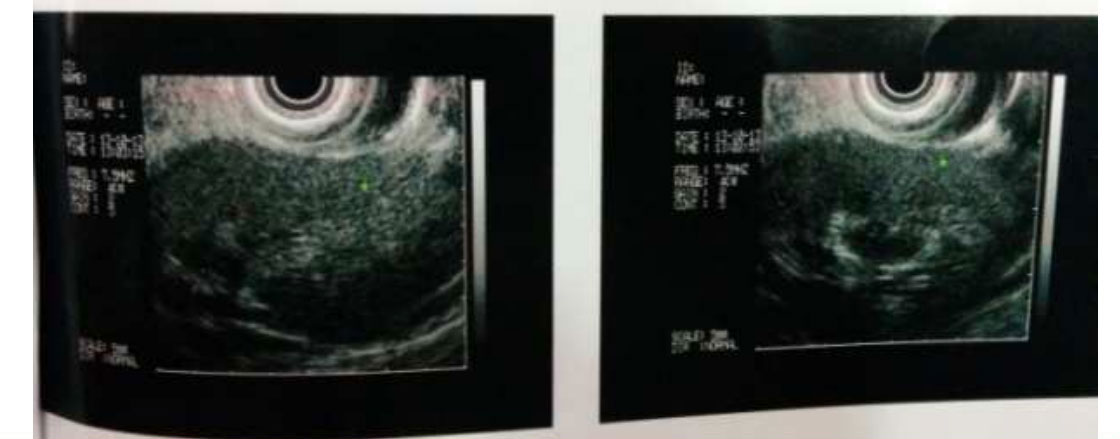
Figure 1: EUS Image showing showing hypoechoic lesion
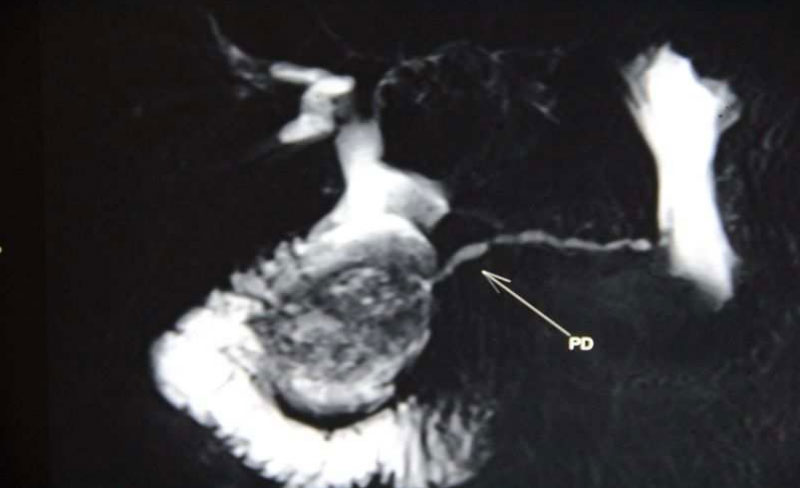
Figure 2: MRCP image - Contrast enhancing lesion with Pacreatic Duct(arrow pointer) opening into it
DISCUSSION:
The term Bile Duct Cysts should be used more often, since the ductal cysts can involve any part of the biliary tract. The diagnosis of bile duct cysts are delayed in upto 20% of patients until adulthood. Several types of choledochal cysts are recognized, they have been classified by Todani into 7 types.[5] The bile duct system anomalies can be broadly classified into: Ductal Plate Malformations (DPM) and Abnormal Pancreatico-Biliary Ductal Junction (APBDJ). DPM is responsible for the intrahepatic version of the bile duct anomalies. APBDJ is a very common occurrence seen in upto 92% individuals (also referred to as ‘common channel disorder’). When the P-B junction is proximal to the sphincter of Oddi, the resultant duct that forms is called the ‘common channel’. An APBDJ is defined as the length of the common channel between the confluence of CBD and PD, and to the Oddi’ sphincter > 15mm.[6] The prevalence of this anomaly varies from 21% – 90%.
The basic anomaly of the disease is the embryological arrest of the pancreatico-biliary junction towards the duodenal wall. The result is the extra-duodenal location of the junction and an abnormally long ‘common channel’.[7] Insufficient flow into the duodenum leads to accumulation of secretions in the common channel, activation of the pancreatic juices, reflux towards the biliary duct system, high pressures and enzymatic action, a probable cascade of events leading to the final pathology.
Initial recognition of the disease is mostly incidental on hepatobiliary imaging. The patient can present to the physician with the following symptom complexes:
- epigastic or right hypochondriac pain, abdominal tenderness
- fever with chills, rigors, associated with anorexia
- nausea and vomiting
- jaundice, occasional biliuria
- rarely, cholangitis and frank sepsis. Cirrhosis associated with portal hypertension, hepatomegaly and splenomegaly are common in such cases
- Pancreatitis.

Figure 3: CECT Image showing Contrast enhancing lesion, CBD cyst close to pancreatic head

Figure 4: CBD cyst specimen cut open, showing pancreatic duct opening it.
Pancreatitisis seen in 30%-70% of cases associated with bile duct cysts; symptoms of pain and vomiting are more severe. In our patient, the symptoms of pain and vomiting were persistent for over 2 months, with intermittent waxing and waning. Presentation of the patient with chronic pancreatitis is extremely uncommon. Yamaguchi (1980) and Jallek & Williamson (1991) reported few cases; the latter reported a case with recurrent acute pancreatitis has at led to chronic pancreatitis. 90% of patients with choledochal cysts having a diameter equal to, or greater than 5cm.[8] The incidence of pancreatitis has also been reported to be much higher in patients with a longer (more than 21mm) and wide common channel (greater than the size of pancreatic duct).[9] The exact cause of pancreatitis in cystic biliary disease in unknown, though an abnormal P-B junction seems to be the centre of the pathology. In our case, a well-formed common duct was noted, but the length and the width were not very large.
Malignancy has been reported to occur in 2.5% - 2.8% of patients with choledochal cysts, a risk of 20 times greater than the general population;[10] chronic stagnation probably leads to the development of carcinogens.
Partial excision of the cyst and Cystenterostomy (internal drainage of the cyst) exposes the patient to risk of cholangitis, pancreatitis (as in our patient) and cholangiocarcinoma. Visser et al described a series of 39 patients. 8 out of them had undergone partial cyst excision, drainage or followed expectant management initially, and 7 out of these were found to have cholangiocarcinoma or gall bladder carcinoma. All the 39 patients were subjected to complete excision of the cyst, none of them were found to have cancer on long term follow-up.[11]
In our patient, abdomen was opened with a bilateral, subcostal ‘rooftop’ incision. Adhesiolysis and Hilar plate dissection was done. The cyst was intra pancreatic in location, involving the infra duodenal part of the CBD. An intra operative cholangioangiogram did not reveal any abnormality of intra-hepatic biliary anatomy. The cyst was indenting on to the C-loop of duodenum. A patent hepatico- duodenostomy was present. The treatment of choice for choledochal cyst is complete excision with biliary-enteric anastomosis. It has been described by various workers with few variations. A Roux-e-y hepaticojejunostomy is preferred to hepatico-duodenostomy due to the higher incidence of duodenogastric bile reflux in the latter.[11]The decision to perform a Classical Whipple's surgery was taken primarily on the following grounds:
- The cyst was ‘inseparable’ from the pancreatic tissue.
- The main pancreatic duct was opening into the cyst (which was confirmed after cutting open the cyst post-excision).
- Proximity of the Cyst to the duodenum and indenting the latter.
The entire Cyst and surrounding pancreatic tissue was excised, after Kocherization of the duodenum. Hilar plate was dissected and duodenum was excised. Jejunal limb of small gut was mobilized. A Gastro-Jejunostomy, Pancreatico-Jejunostomy and Hepatico-Jejunostomy was performed, followed by a feeding jejunostomy. The opening of the pancreatic duct into the cyst was clearly demonstrable on opening the cyst.
The patient recovered well from the surgery over the next 7 days and was discharged home on normal diet. Histopathology exam confirmed a Type 1 Choledochal cyst with mild chronic inflammatory changes. The cyst wall showed lymphoplasmacytic cellular infiltration with lymphoid Hyperplasia. There was no evidence of malignancy in the cyst wall or surrounding pancreatic tissue.
CONCLUSION:
Several workers have reported mere internal drainage of the cyst with good results. But the present evidence dictates complete excision of the cyst in view of malignant degeneration. Intraduodenal cysts, such as in our patient, in close association with pancreatic-biliary junction demand a Whipple’s procedure.
REFERENCES:
- Lu S: Biliary cysts and strictures, in N Kaplowitz (eds): Liver and Biliary Diseases, Baltimore, MD, Williams and Wilkins, 1996, pp 739-753.
- Lipsett P: Biliary atresia and cysts, in Pitt H (eds): The Biliary Tract (part of Clinical Gastro Enterology). London, UK, Balliere Kindall, 1997, 11 (4), pp 626-641.
- Vater. Dissertation in auguralis medica, poes diss. Qua Scirris viscerum dissert, c.s. ezlerus. Edinburgh : University Library, 1723.
- Douglas A. H. Case of dilatation of the common bile duct. Monthly J Med Sci (Lond), 1852, 1497.
- Cushieri A. The Biliary tract In.: Cushieri A, Giles GR,Moosa AR. Essential surgical practice, 3rd Ed,1995, 968-969.
- Babbitt DP, Starshak RJ, Clemett AR. Choledochal cyst: a concept of etiology. Am J Roentgenol Radium Ther Nucl Med 1973; 119:57-62.
- Congenital dilatation of Common Bile Duct. Srp Arh Celok Lek, 2001 May-Jun; 129 Supple 1: 47-50.
- Swisher SG, Cates JA, Hunt KK, Robert ME, Bennion RS, Thompson JE, et al. Pancreatitis associated with adult choledochal cyst. Pancreas 1994 ; 9:633-7.
- Komuro H et al. Pancreatic complications in choledochal cysts and their surgical outcomes. World J Surg 2001 ; 25:1519-23.
- Tan S S, Tan N C, Ibrahim S, Tay K H. Management of adult choledochal cyst. Singapore Med J 2007; 48 (6) : 524.
- Emedicine.medscape.com/article/172099- treatment:2.