Liver Disease

Hepatobiliary Disorders Requiring Surgery
Hepatocellular Carcinoma (HCC)
A primary liver cancer seen mostly due to alcohol, Hepatitis B and C. Almost 80% are unresectable due to advanced cirrhosis or extra hepatic disease. Till date liver resection is the mainstay of the therapy and ranges from segmentectomies to major lobar resection based upon the size & location of the tumour as well as the volume & quality of theresidual liver. Local ablative procedure like radiofrequency ablation is done mainly for smaller tumors where in a resection cannot be done for various reasons. Other therapies like chemoembolization ,radioembolization and portal vein embolization may be required on case to case basis. Median 5 years survival for resected patients is about 30%. A small subset of patients are candidates for Liver transplant.
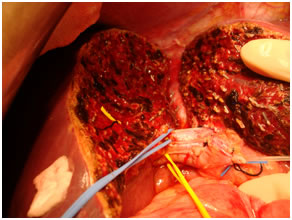
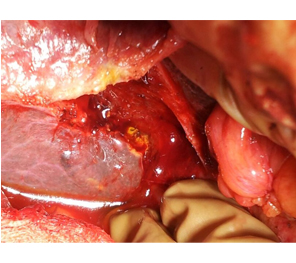
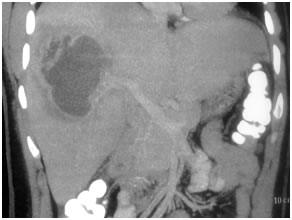
HCC in a non cirrhotic liver

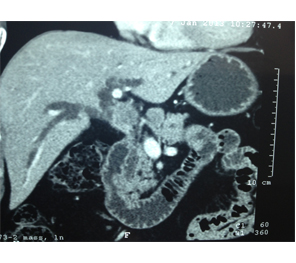
Large HCC in seg 2 & 3
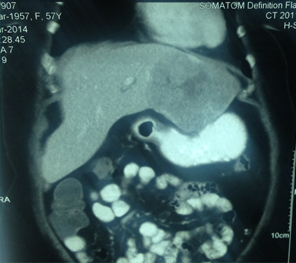
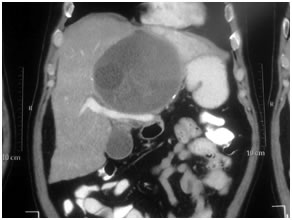
CT Scan showing Lipoidol uptake in segment VIII

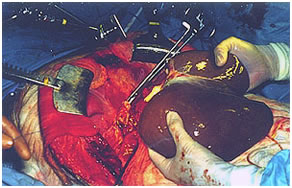
Intra Operative image after right hepatectomy

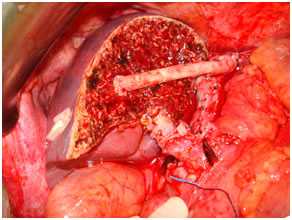
Specimen of bisegmentectomy, Segment V & VIII

Hilar Cholangiocarcinomas( Klatskintumors)
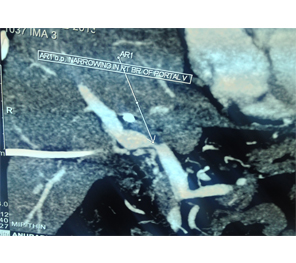
These biliary tumors affect the junction of the right and left hepatic ducts sometimes infiltrating the adjacent liver and surrounding vascular structures. Patients are usually jaundiced at presentation and may require drainage by PTBD to reduce bilirubin esp if liver resection is being planned. Portal vein embolization may be required for future liver remnant hypertrophy to prevent liver failure. Median 5 years are approximately 25 %.
Surgery involves Hepatectomy with caudate lobectomy along with excision of the extrahepaticbileduct& lymphadenectomy of the Hepato duodenal region. It also entails a Hepatico jejunostomy on the opposite side.
With growing experience we have managed advanced disease particularly with vascular involvement& refused by other centres with good results.
Rt Hepatico-jejunostomy

Hilar CC after resection
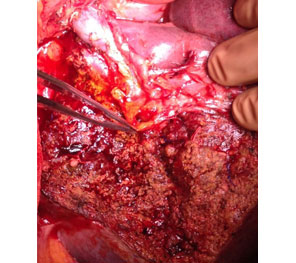
Type 3b resected specimen

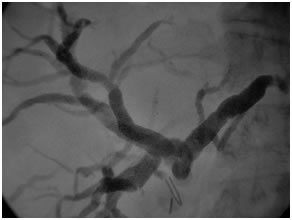
Vascular narrowing of R PV in type 3b
Separate R & L ducts
Type 2
ERCP showing type I hilar block

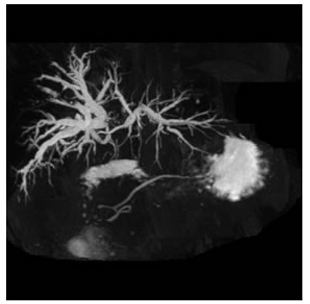
MRCP showing type III b hilar tumor
Specimen of radical bile duct excision

Specimen of resected hilarcholangiocarcinoma

Post Cholectystectomy Biliary Strictures
These usually stem from a poorly performed cholecystectomy (Lap/open) either because of a difficult anatomy or an overconfident surgeon or a combination of both! Associated vascular injury makes matters worse. The presentation may be in the early postoperative phase (patient usually jaundiced) with or without a bile leak or much later as a cicatrical stricture (again patient jaundiced). Reconstructive biliary surgery remains the gold standard where a Roux-en Y Hepatico jejunostomy is done. We generally advocate a prior PTBD for a road map & easier identification of ducts as well as a PTBD gram for documentation of the anastomosis.
PTBD gram showing biliiary leak

PTBD gram showing type II biliary stricture
Intra Operative picture of Hepatico Jejunostomy

Post operative PTBD gram showing a patent high hepaticojejunostomy

Haemangiomas:

There are the commonest space occupying lesions (SOL) of the liverthe others being
- Metastasis
- Hydatid cysts
- Liver abscess
- Adenomas
- Focal Nodular hyperplasias(FNH)
Heamangiomas are benign lesions and generally warrant no therapy unless symptomatic. Lesions greater then 10cms are termed Giant haemangiomas and may cause symptoms like pain and organ compression leading to jaundice (bile duct) or vomiting (stomach). In such cases resection is required to relive the symptoms.
Liver Abscesses
These are benign liver lesions that are seen not so infrequently. Liver abscesses can be amoebic (protozoal) or pyaemic (bacterial). Both have generally a dramatic presentation with patients having fever, pain in upper abdomen, elevated blood counts. USG / CT Scan are diagnostic. Treatment generally involves antibiotics & metronidazole. Percutaneous aspiration is done for large abscesses or those that are not resolving. Surgery (open/laparoscopy) is required for drainage of ruptured abscesses in the peritoneal cavity.
Hydatid Cysts
Hydatid cysts occur due to transmission of EchinococcusGranulosus (tapeworm) from pets through the faeco oral route. Most patients are asymptomatic wherein the cysts are detected incidentally. Dead cysts generally are calcified. Most have daughter cysts within them. Surgery is the gold standard & ranges from opening the cyst under sterile scolicidal precautions & removal of the germinating membrane, packing the cavity with omentum& under-running bile leaks if any, to cysto-pericystectomy to hepatectomy. A course of Albendazole is given for atleast 6 weeks.
Amoebic Liver Abscess
Hydatic Cyst in Liver
Gallbladder containing daughter cyst

Liver Transplantation
Liver transplantation (LT) is today an established mode of therapy for end-stage liver disease. Although it is more than 40 years since the first Liver transplant was performed it is only in the last few years that this modality has made inroads in our country. It is a complex, expensive yet life saving procedure.
Common indications include cirrhosis, hepatocellular cancers (only those meeting specific criteria), metabolic disorders, Fulminant liver failure & biliary atresias in the pediatric age group.
Liver transplantation can be Deceased donor wherein the liver is procured from a brain dead individual or Living donor where only a part of the liver sufficient enough to meet the metabolic demands of the recipient is harvested from an immediate relative. Living donor transplant is more complex than the conventional method as it entails doing a partial hepatectomy on a person (donor) who otherwise is healthy & is disease free! Of course, life long immunosuppression is mandatory to prevent rejection of the new liver.
Successful Liver transplantation requires an integrated team effort comprising of the surgeon, hepatologist, intensivist, radiologist, pathologist, transplant co-coordinator & ancillary services.
Deceased Donor Liver transplant
Living Donor Liver Transplantation
Living Donor Hepatectomy