Pancreatic Diseases
Periampullary And Pancreatic Cancers

These are disorders of the 5th and 6th decade though occasionally we have seen these in the 3rd decade as well. Diabetes is considered a risk factor as also Familial Adenosis Polyposis. Jaundice (obstructive in nature) is the most common presenting feature of these cancers. The formidable Whipple's procedure (Pancreaticoduodenectomy) is the mainstay in trying to achieve a cure for these cancers. It entails removal of the head of the pancreas, the bile duct and Gall bladder, duodenum & at times a small part of the stomach.
Reconstruction is done by a Pancreatico-jejunostomy preferably a duct to mucosa, biliary enteric & a gastro-jejunostomy for continuity. Our large experience & increasing numbers have led to lowering of the mortality (5%) over the years. The pancreatic leak rate has also reduced to around 12%. Five year survivals vary from 15% to 50% depending on the type of pathology.
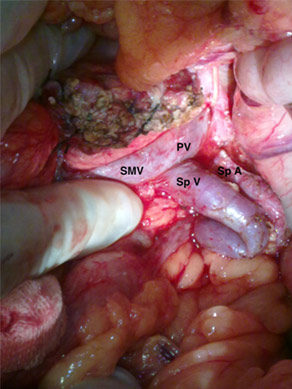
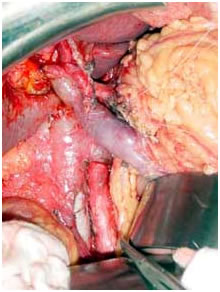
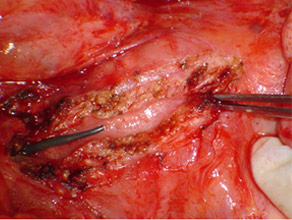
Intra operative photo after radical resection
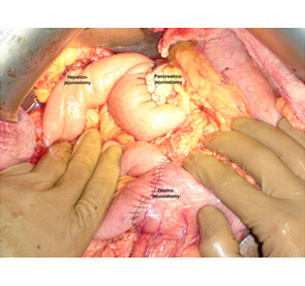
Intraoperative photo showing all the anastomosis
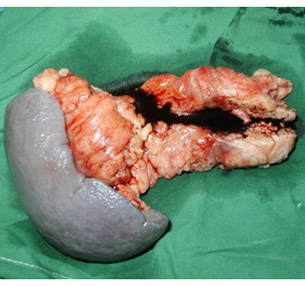
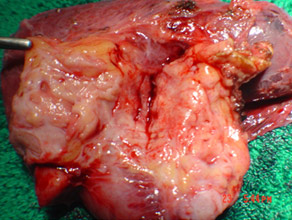
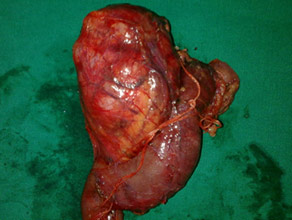
Specimen photo after radical resection for pancreatic cancer

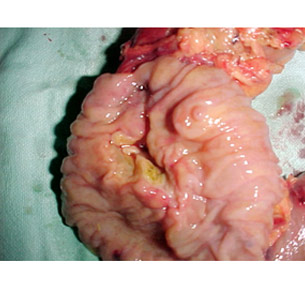
Resected specimen after Whipple's procedure

Resected specimen showing ampullary cancer
Whipple for Pancreatic Neuroendocrine tumor

Specimen of distal pancreatectomy spleenectomy for cancer
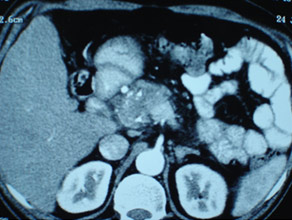
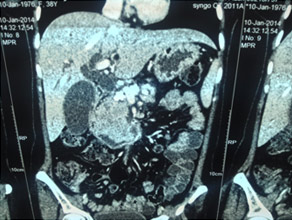
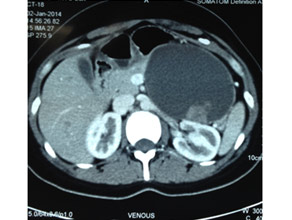
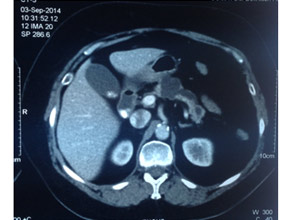
CT scan of pancreatic cancer in the body

Large Neuroendocrine tumour in pancreatic head

Acute Necrotizing Pancreatitis (ANP)
ANP is a clinical condition affecting not only the pancreas but other organ systems as well. It can be a dreaded and severely life threatening condition if timely therapy is not instituted. The inherent mortality of this condition again has fallen from 40% to 15% in our centre. Initial therapy of recussitation& conservative management of SIRS needs to be done in an ICU to tide over the first couple of weeks. Intervention (Radiological or Surgical) is requiredto tackle infected Acute Necrotic Collection (ANC) or Walled Of Necrosis (WON).Surgical intervention is generally delayed to atleast 4 weeks if possible so that the necrotic elements separate from the viable pancreas. At times a second or third debridement may also be required albeit rarely.
Common causes include gallstones, alcohol abuse, hyperlipidaemias and idiopathic.
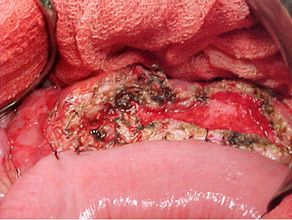
CT Scan of Infected Pancreatic necrosis

Necrotising pancreatitis Cast

Necrotising pancreatitis specimen(infected)

Chronic Pancreatitis:
A continuing inflammatory process characterized by irreversible morphological change typically causing pain and loss of function. Common causes include chronic alcohol abuse, hyperlipidaemia, hypercalcaemia, malnutrition, tropical and idiopathic. Commonest mode of presentation is chronic pain (upper abdomen and back) and may be associated with Diabetes Mellitus and steatorrhoea (loose oily stools). Importantly pancreatic cancer may occur in 3%-18% of these patients. Surgery tackles pain & surrounding organ complications like duodenal and biliary obstruction secondary to a pancreatic head mass. Surgery varies from a simple pancreaticojejunostomy for Pancreatic duct drainage to the more complex head coring procedures (Frey’s and Beger’s procedure). The radical Whipple’s procedure is done when cancer cannot be ruled out.
Surgical results for pain relief varies between 75% to 90% at 5 years.
As against Endotherapy surgery is a one off procedure tackling other issues like biliary stricture (which are often resistant to endotherapy) as well as pancreatic head masses which need surgical decompression for pain relief.
Chronic pancreatitis with large pseudocyst

Opened pancreatic duct with stent inserted proximal to the stricture (forceps)
Pancreatico-jejunostomy: a standard procedure
CT of pancreatic head mass showing stipled calcification
CT scan of pancreatic head mass

Freys head coring for a large pancreatic head mass (benign)

Beger's head coring (pancreatic neck is split exposing the vein)

CT scan of Chronic pancreatitis with cancer (stent seen in the pancreatic duct, arrow pointing the tumor)

CT scan of chronic pancreatitis with large tumor, stones in the pancreatic duct
Chronic pancreatitis with cancer(specimen)
Chronic pancreatitis with fungating tumor (specimen)

Cystic Tumors Of The Pancreas:
These are not so unusual and are at times mistaken for pseudocysts. In fact 30% of treated pseudocysts are actually tumors. Tumors vary from the benign serous cystadenomas to locally aggressive and potentially malignant mucinous and solid pseudopapillary tumors. Surgical resection of the tumor is necessary as these can undergo a malignant change.
Not all cystic lesions require surgery,infact a fair of them can be observed for their progression. Surgery may be necessary in large tumors which cause symptoms such as pain, jaundice and at times pancreatitis due to ductal obstruction.
Conservative surgery when possible is the norm. Saving the parenchyma as in Central pancreatectomy or vessel & spleen preserving pancreatic resections are the norm now for low grade/borderline lesions.
CT scan of a Solid pseudopapillary tumor in pancreatic body

CT scan of large mucinous cystic tumor with a solid component in pancreatic body
Specimen of Solid pseudopapillary tumor in pancreatic body

Specimen of Large cystic tumor in pancreatic body

CT scan of Solid pseodopapillary tumor in pancreatic head

Large solid pseudopapillary tumor in pancreatic head (specimen of Whipples)
CT scan of main duct Intraductal Papillary Mucinous Neoplasm (IPMN)
Central pancreatectomy specimen of Main duct IPMN

Vessel and Spleen preserving pancreatectomy